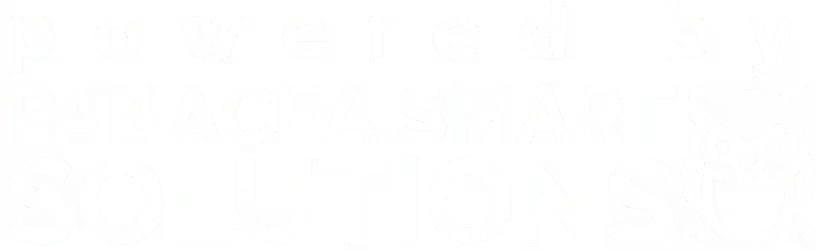
Medical billing in the orthopedic field is a challenging process because it includes various procedures, treatments, and surgeries. Efficient orthopedic medical billing solutions help providers to streamline their RCM process and improve cash flow. It ensures providers are getting accurate and timely payments for their services.
This blog covers what orthopedics is, why it matters, common challenges, and the best practices to get faster reimbursements.
Understanding Billing in Orthopedic Services
Orthopedics is a branch of medical care that is concerned with musculoskeletal conditions. It involves the treatment of joints, bones, tendons, ligaments, and more. Orthopedic billing services play a vital role in completing the complicated processes accurately and meeting strict rules and regulations. Here, an efficient medical billing and coding practice is essential to avoid costly mistakes for the service already provided.
What Does Orthopedic Billing Services Include?
Billing services for an orthopedic service cover several tasks that are important for timely reimbursement. It involves verifying the patient’s eligibility, accurate documentation, and medical coding, submitting the claims, and managing denials. Some of the key components are detailed below-
Insurance Verification
Confirming whether the patient’s insurance covers the orthopedic service or not.
Accurate Coding & Documentation
Specialized coders use orthopaedic CPT codes for procedures, ICD-10 codes for diagnoses, and HCPCS codes for supplies. It ensures precise documentation for supporting the codes.
Claim Submission
This step includes submitting a clean claim to the insurance company on time.
Denial Management
The orthopedic medical billing companies identify the reasons behind the denial and then resubmit the corrected claim.
Payment Posting & Reconciliation
It involves posting the payments received from insurance companies accurately. Then, reconciliation with submitted claims to determine any discrepancies.
Patient Billing & Collections
Managing patient billing inquiries and generating statements.
Revenue Cycle Management (RCM)
Some of the best Orthopedic Medical Billing companies, like panaHEALTH, provide complete RCM services. Offering end-to-end support from patient registration to claim resolution.
Compliance & Regulatory Adherence
Ensuring compliance with all necessary regulations, which include HIPAA and payer-specific guidelines.
Common Mistakes Made in Orthopedic Billing Practice
The most common orthopaedic coding and billing mistakes involve filling in incorrect patient information and documents, improper coding, not getting pre-authorizations, and missing deadlines. These errors result in claim denials, legal issues, and delayed payments. Explore the Detailed Explanation of Common Billing Mistakes-
Failure to Verify Insurance
Confirming your patients’ eligibility at the initial stage is important to reduce any financial risk. It leads towards a smoother claim process and higher reimbursements.
Incorrect Patient & Insurance Information
Errors in filling patients’ demographics, like name, date of birth, etc, and insurance details are the most common reasons for claim denials.
Coding Errors
Errors in orthopedic coding are one of the major reasons for claim denials. It can occur in the following terms:
Incorrect ICD-10 codes: Incorporating inappropriate or outdated diagnosis codes.
Unbundling: Using separate codes for medical procedures that need to come under a single code.
Upcoding/Downcoding: using high or low-level codes that are not appropriate for the provided service.
Incorrect modifiers: Missing or inaccurate modifiers lead to claim denials.
Lack of Documentation
Detailed documentation is important to support modifiers.
Timely Filing Deadlines
Not submitting claims before a specified time period results in claim denials. Usually, the timeframe is between 90-180 days from the date of service provided.
Explore the Best Orthopedic Billing Practices
An effective RCM process is essential for every orthopedic practice. Adopting the best orthopedic medical billing practices helps to accelerate reimbursement and strengthen a practice’s financial health. Deep dive into the top techniques for faster and smoother billing.
Capture Accurate Patient Information
Most importantly, the patient details ( demographics, insurance data, medical history, contact info) need to be filled in accurately. Build a double‑verification strategy and leverage digital forms to reduce manual entry errors.
Document All Medical Necessity Clearly
Insurance companies require various documents that justify the need for procedures. In orthopedic billing, it is important to share every detail about the patient’s condition, tests, symptoms, and selected treatment.
Submit Claims Promptly
Timely claim submission matters a lot. Make sure to complete the entire billing process and submit the claim within 24 to 48 hours of service provided. Set an internal deadline for every practice, monitor the claim status frequently, and ensure submission on time to enhance cash flow.
Ensure Prior Authorization
In most cases, orthopedic procedures demand prior authorizations that vary across payers. Make sure authorization is obtained in advance to avoid any denial and claim rejection.
Leverage Advanced Billing Software
Look out, orthopedic billing services that utilize advanced software integrated with your EHR. These systems offer claim‑scrubbing tools, coding assistance, and other essential features. This kind of automation helps in reducing errors, supporting data flow, and speeding up the process.
Stay Informed with CMS Updates for Orthopedic Billing
Accurate CPT, ICD‑10, and modifier use are crucial. Partner with the right orthopedic medical billing company to use the latest codes and meet the evolving regulations. Explore the latest CMS Updates for Orthopedic Billing.
- New Prior Authorization Requirements
Now, CMS has expanded prior authorization requirements for some of the high-cost orthopedic treatments. These are-
- Total Knee Arthroplasty (TKA) – CPT 27447
- Total Hip Arthroplasty (THA) – CPT 27130
- Spinal Fusion Surgery – CPT 22612, 22630
- Bundled Payments & Episode-Based Care Expansion
CMS has expanded bundled payment models for joint replacement surgeries, fracture management, and spinal procedures. The orthopedic biller now needs to document all services correctly within an episode of care to get the full reimbursement.
- Modifier 25 & 59 Restrictions
- More strict guidelines for Modifier 25 (a procedure-billed E/M visit)
- When doing different treatments on the same day, Modifier 59 needs to be used carefully.
- Extension of Telehealth Coverage for Orthopedic Follow-Ups
- Telehealth is now reimbursed by CMS for physical therapy and post-operative visits.
- E/M follow-ups (CPT codes 99212–99215) are covered for remote patient monitoring.
Get the Best Orthopedic Billing Services
The success of orthopedic billing practice depends on accurate and timely claim submission. Any kind of error can result in rejected claims and revenue loss.
Given the challenges of the process, it’s a great idea to outsource to a trusted orthopedic billing company. One such company is panaHEALTH solutions, which provides your complete RCM support, including active services, Orthopedic Medical Billing and Coding Services, denial management, and AR solutions.
Reach out today to reduce denials and enhance your collections.